
A baby is born with diffuse, red, scaly skin, erosions and blisters. Later the skin becomes hyperkeratotic. Mom has the same condition.

A baby is born with diffuse, red, scaly skin, erosions and blisters. Later the skin becomes hyperkeratotic. Mom has the same condition.
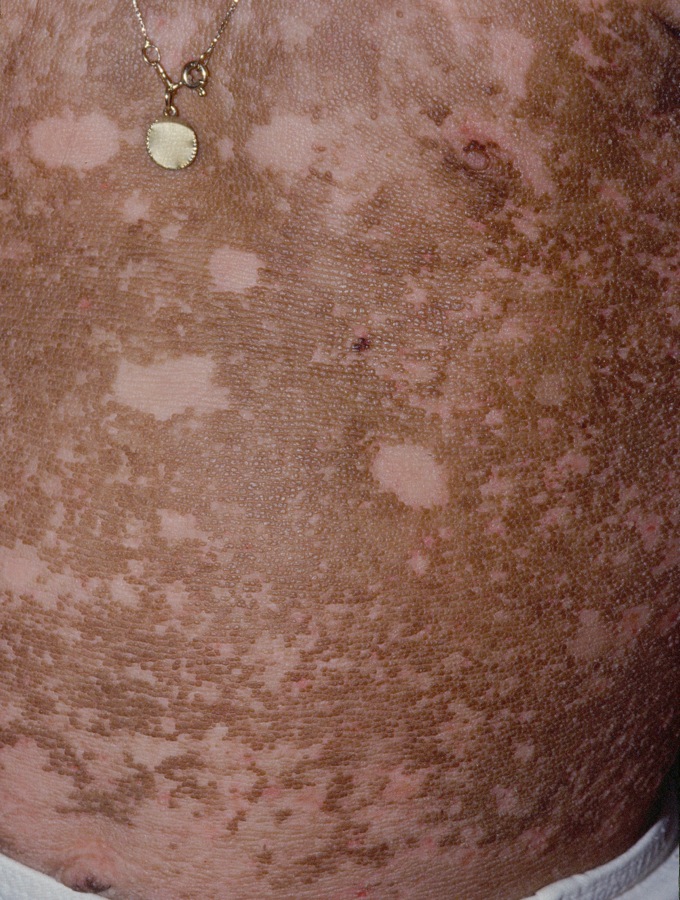
Areas of denudation and later normal skin adjacent to verrucous areas is typical.
Epidermolytic hyperkeratosis (EH), also known as bullous congenital ichthyosiform erythroderma, is an autosomal dominant genodermatosis caused by defects in keratins 1 and 10.
Inheritance is AD. Approximately half of the cases are sporadic without any family history. Defect in the genes that code for keratins 1 and 10 have been found. Patients with epidermal nevi which histologically show epidermolytic hyperkeratosis may give rise to offspring with classic, diffuse EH if the post zygotic mutation is present in the gonads.
The affected infant will have diffusely red, scaly skin with blister formation and/or erosions (which gave rise to the former name of bullous icthyosiform erythroderma). Later, patients develop ichthyotic, verrucous and hyperkeratotic lesions which persist for the rest of the patient's life. Areas of denudation and later normal skin adjacent to verrucous areas is typical. The palms and soles are common areas of verrucous huyperkeratosis. Bacterial overgrowth and macerated skin can give rise to a pungent odor. Various subtypes of EH have been described, notably those with and without palmoplantar involvement. Unilateral cases have been described.
Annular Epidermolytic Ichthyosis is a milder variant where the symptoms improve in the first year of life and polycyclic red, scaly plaques appear.
Ichthyosis bullosa of Siemens is a rare, autosomal dominant, blistering ichthyosis similar to epidermolytic hyperkeratosis, except that hyperkeratosis is mild, the epidermolysis involves mostly the granular layer and is less extensive, and the gene defect is keratin 2e.
Homepage | Who is Dr. White? | Privacy Policy | FAQs | Use of Images | Contact Dr. White